Obstetric Anesthesia and a Scorecard for Newborns, 1949-1958
During her tenure as division director, Apgar became increasingly aware that obstetric anesthesia was a neglected area, partly because her division took on much of the obstetric anesthesia work at Presbyterian during the war. By the 1930s more babies were being born in hospitals than at home, and yet maternal and infant mortality in America was still considerably higher than in many European countries. Infant mortality figures overall improved between 1930 and 1950, but the mortality rates for the first 24 hours after birth changed hardly at all. Relieved of the demands of administration, Apgar focused her teaching and research on this problem.
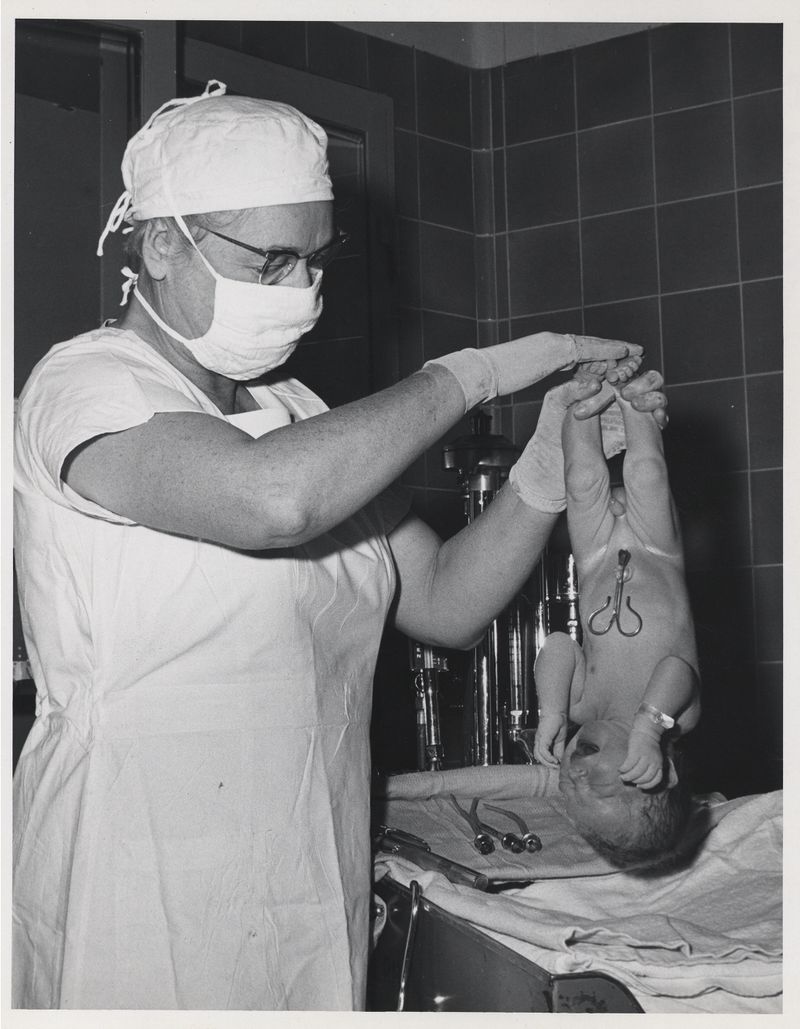
It became clear to Apgar that in many cases, newborns could be saved if anyone bothered to examine them closely just after birth. Oxygen lack (anoxia) played a major role in at least half of newborn deaths; why was the obvious remedy--getting oxygen into the baby--not widely applied? Trained medical anesthesiologists were not always present in the delivery rooms, because there were not enough anesthesiologists available. The delivery-room staff were usually focused on the mother, so that junior medical residents, with only rudimentary training or experience in resuscitation, often were given responsibility for the newborn. Few residencies required any training in anesthesia, and little had been written about obstetrical anesthesia. What training the residents did receive often emphasized certain types of equipment or stimulating drugs, rather than the basic principles of prompt action, maintaining a free airway, and getting oxygen into the baby.
Besides this, Apgar noted, resuscitation of infants at birth was a topic fraught with strong opinions, imaginative ideas, and unscientific studies. There was little agreement about what was "normal" just after birth, and when intervention was needed. Some practitioners kept track of "breathing time," defined as the time from delivery of the head to the first respiration, or "crying time," the time until the establishment of a satisfactory cry. Others used the terms "mild," "moderate," and "severe" depression to describe the infant's condition. As Apgar observed, these indicators had serious flaws: if the mother received high doses of depressant drugs during labor, it was common for the baby to breathe once, then stop breathing for many minutes, making it hard to determine the "breathing time." Some infants don't cry for a long time after delivery. Terms such as "mild, moderate, and severe depression" left a fair margin for individual interpretation.
Apgar had little patience with these ideas. It might be difficult to discern a baby in trouble during the delivery process (fetal monitors were not available until much later on), but once the baby was born, problems were often obvious: an infant who was not breathing, breathing feebly, or with occasional deep gasps needed oxygen. Pale or bluish skin tone, limpness, or slow heartbeat merely underscored this need. It should be routine, Apgar believed, to handle such infants by first clearing the airway, then proceeding to mouth-to-mouth or mask administration of oxygen. Once she entered obstetric anesthesia in 1949, she set out to ensure that newborns received more attention. As a first step, anesthesia residents at Presbyterian began doing required rotations in obstetrics.
The Apgar Score, as it later became known, had its origins in a medical resident's question: How would one do a standard, rapid assessment of a newborn's condition? Apgar responded, "That's easy, you would do it like this." Grabbing the nearest piece of paper, she jotted down five objective points to check: 1) heart rate, 2) respiration, 3) muscle tone or activity, 4) reflex response to stimulation, and 5) color. These were the standard signs monitored by anesthesiologists during surgeries. During the next year Apgar developed the five points into a scoring system for newborns, to be used not just for determining the need for resuscitation, but as a "basis for discussion and comparison of the results of obstetric practices, types of maternal pain relief, and the effects of resuscitation."
Each of the five signs, observed one minute after birth, was rated 0, 1, or 2, depending on whether it was absent or present. A score of 10 indicated a baby in the best possible condition.
0 1 2
Heart rate Absent < 100 per minute 100-140 per minute
Respiration Absent Irregular Strong, crying
Reflex Irritability Absent Weak Grimace, sneeze
Muscle tone Flaccid Some flexion Strong flexion
Color Blue Extremities blue Pink
In September 1952 at the Twenty-Seventh Annual Congress of Anesthetists, Apgar presented the results of a trial of the scoring method used on 1,021 infants born at the Sloane Hospital for Women at Presbyterian. The trial showed correlations between infant scores and method of delivery (spontaneous, forceps-assisted, caesarian, etc.) and the type of anesthesia used on the mother. The now-classic study was published the following year, titled "A Proposal for a New Method of Evaluation of the Newborn Infant." Although other practitioners experimented with scoring at five minutes, ten minutes or longer intervals after birth, Apgar maintained that the one-minute score was the most immediately useful, providing a rapid evaluation of the infant at a time when its physiological state can vary quickly from healthy to severely depressed. (Most hospitals now score at one minute and again at five minutes after birth.) She also recommended that scoring be done by someone other than the attending obstetricians, who, she discovered, almost always rated "their" infants several points higher than did other members of the delivery team.
During the next six years, Apgar and her colleagues scored thousands of infants, and correlated the scores with other clinical factors. They discovered that while newborn blood oxygen levels did not correlate with low scores, levels of carbon dioxide and blood pH did: infants with scores of 3 or less were almost always in a state of respiratory and metabolic acidosis, and in need of resuscitation. They also looked at how newborns were affected by the type of anesthesia given to their mothers during the delivery, and found that general anesthesia, especially cyclopropane, seemed to exacerbate newborns' asphyxia, while regional anesthetics did not (though both types crossed the placental barrier). The scores served as the basis for studies on newborn respiration and physiology, and the studies in turn validated the scoring system's utility. These studies also elucidated many aspects of maternal-fetal metabolism that were poorly understood before.
As the scoring method was made standard at Presbyterian's Sloane Hospital, and adopted at other medical centers, data was collected on thousands more infants. This allowed Apgar and her co-workers to build much better statistical pictures of what was happening in the delivery rooms, and how all sorts of variables might affect a newborn's chances for survival. While the score could not be used to predict the survival of individual babies, it could be shown that in general, full-term newborns with good scores (7-10) had a significantly better chance of surviving their first month of life.
By the early 1960s, many hospitals were using Apgar's scoring method. In 1961, Dr. Joseph Butterfield at the University of Colorado Medical Center in Denver wrote to Apgar with the news that one of his residents had used the letters of her name as a mnemonic device for the five scoring criteria:
A- Appearance (Color)
P- Pulse (Heart rate)
G- Grimace (Reflex irritability)
A- Activity (Muscle tone)
R- Respiration
Apgar was delighted with the epigram, and it was rapidly adopted. New users of the method (and parents of newborns) often didn't realize that the Apgar Score was actually named for a person. As she told Butterfield, Apgar was once greeted by a secretary at a Boston hospital, who said, "Oh, I didn't know Apgar was a person; I thought it was just a thing!"